Every question you’ve ever had about sexual health, answered by the experts.

Ever had a question you’ve been too embarrassed or afraid to ask about sexual health? Fear not, for Rife magazine has done all the asking for you! So, in the words of Salt-n-Pepa; Let’s talk about sex
Recently Brook , a national charity that provides sexual health and contraceptive advice and services for young people, approached Rife about collaborating on an article about sexual health. I reached out to my Facebook friends and asked them which questions about sexual health they’ve always wanted answered. The answers to these questions were handily provided by the team at Brook in Bristol with some help from their partners at UNITY.
Is sex supposed to hurt?
No. Sex is not supposed to hurt.
Sometimes if you are having penetrative sex for the first time this can be uncomfortable, or penetrative sex without sufficient lubrication can cause discomfort. But as a rule, sex should not hurt, sex should be pleasurable.
If you are experiencing discomfort or pain during any sexual activity it is a really good idea to pause any sexual activity and have a conversation with your partner. It could be that changing position, adding lubrication (water based lube can be easily purchased at pharmacies/supermarkets or can be obtained for free from sexual health clinics), or changing the type of sexual activity can fix the issue. But always remember to check in with yourself too. Do you want to be having sex right now? Does this feel good for you? If you’re unsure about the answer to either of these questions then stop the sex and have a conversation with your partner.
If you are experiencing any pain after sex or any bleeding after sex then it is always a good idea to pop down to your local sexual health clinic to get checked as it can sometimes be an indication of an underlying issue.
What training do sexual health clinic staff receive for trans patients?
Training around trans-specific sexual health issues is becoming more prevalent in healthcare, and there is also more research being conducted into trans people’s health.
At Brook we work hard to ensure our service is as inclusive as possible and that we are up to date on issues facing the LGBTQ+ community both in their personal lives and wider society. Members of Brook attend LGBTQ+ training provided by UNITY sexual health in Bristol, and we in turn deliver LGBTQ+ inclusive sex and relationships training to professionals working with young people, which includes non-binary and gender diverse people.
Brook and UNITY sexual health aim to be as inclusive as possible to all young people who access our services regardless of sexual orientation, gender identity or gender performance, but we always encourage and welcome feedback on how we can improve. If you have any suggestions please email: communications@brook.org.uk or message us on Instagram
How can I have safer sex in non-conventional relationships – I mean polyamory, or even just casual partners?
Having multiple partners can make people more vulnerable to things such as sexually transmitted infections (STIs). It is important for anyone in a sexual relationship to take responsibility for their sexual health, and their partner’s. Here are some suggestions for ensuring that you stay safe:
Have open, honest conversations with your partner(s) about your current relationship structure, your chosen contraceptive methods and any recent sexual activity so that you can both make fully informed decisions about any sexual activity you wish to do together.
- Get STI checks more regularly. This regularity will vary from person to person, but a good rule of thumb is to get checked before every new partner enters your relationship dynamic, as well as a regular check every 6 months – 1 year (like a sort of sexual health MOT). If you want to find out where your local Brook clinic is check out: https://www.brook.org.uk/find-a-service and for UNITY sexual health check out: unitysexualhealth.co.uk/our-services/unity-clinics-opening-times
- Use barrier methods of contraception (such as condoms or internal condoms) for all sexual activity and avoid unprotected sex. Some polyamorous people choose to be ‘fluid bonded’ (having sex with someone without a barrier method such as a condom, internal condom or a dam) with one partner and use barriers with others. Some people choose to use barriers with all their partners.
- For any new partners you can use a ‘sexual health elevator pitch’ which is usually recommended to include the following:
- When were you last tested, what were you tested for, and what were the results? (include any treatment info as appropriate)
- What are your relationship arrangements (are you polyamorous for example) and your relationship status (e.g. I have a wife but we have an open arrangement when it comes to sex) as well as any other information the other person might need to know so they can get to know you a little better (e.g. I use male pronouns or I identify as bisexual)
- What are your safer sex protocols (we need condoms for this, dams for this etc.)
This will help you and your partner(s) make fully informed decisions about any sex and can even be fun (you could even do it in the style of an elevator pitch!)
You can find out more information about the elevator pitch here.
How common are STIs?
Latest statistics from Public Health England show that young people under 25 continue to be most at risk of STIs, along with men who have sex with men.
In 2018, there were 447,694 diagnoses of sexually transmitted infections (STIs) made in England, a 5% increase since 2017.
Chlamydia is the most common bacterial STI diagnosed in England. In 2018 131,269 young people were diagnosed with chlamydia. 60% of new chlamydia diagnoses were in 15-24 year olds – an increase of 2% since 2017. Many STIs including chlamydia, don’t have any obvious signs or symptoms (or they may be so mild they are not noticed) so it is really important to get yourself tested regularly.
Rates of syphilis have also increased both nationally and in Bristol. In the UK there were 7,541 new diagnoses in 2017, a 5% increase from 2015. While the diagnoses numbers are not as large as for other STIs, this represented the biggest increase of any STI in 2015. The picture is looking similar in Bristol.
There were 56,259 diagnoses of gonorrhoea reported in 2018, which is a 26% increase from 2017. There have also been issues with strains of gonorrhoea developing resistance to certain types of antibiotics, although these strains are still treatable it is important to prevent transmission of STIs as much as possible to help combat this problem. The best way to prevent getting a sexually transmitted infection is to use barrier methods of contraception for all sexual activity (condoms or internal condoms for penetrative sex, dams or condoms for oral sex).
What treatments are there for different STIs?
There are a wide range of treatments available for different STIs, and it is important to follow the advice of a medical professional.
Bacterial STIs (this includes infections such as chlamydia, gonorrhoea, syphilis and trichomoniasis vaginalis) are generally treated with a course of antibiotics.
Viral STIs (this includes genital warts, genital herpes and HIV) are treated with a range of anti-viral treatments. Although they cannot be ‘cured’ in the same way that bacterial STIs can, the treatments often remove all symptoms, so combined with careful contraceptive choices people can enjoy fulfilling sex lives.
Parasitic STIs (this includes public lice or “crabs”, and scabies) can usually be treated with creams and lotions to the whole body from the neck down (in the case of scabies) or just to the affected area (in the case of public lice). Some treatments require you to repeat them after 3-7 days. It is best to get the advice of your health professional on this. There are also other recommended steps that go alongside treatment to prevent re-infection including washing your clothing, bedding and towels on a very hot cycle (60C or higher) to kill off any lice and their eggs.
If you think you might have an STI or have come into sexual contact with someone who might have one, it is always important to go and get yourself tested even if you don’t have any symptoms. Remember not to panic, it’s more common than you think and help is always available at your local sexual health clinic.
Information sourced from:
Is there any contraception that is fail-safe?
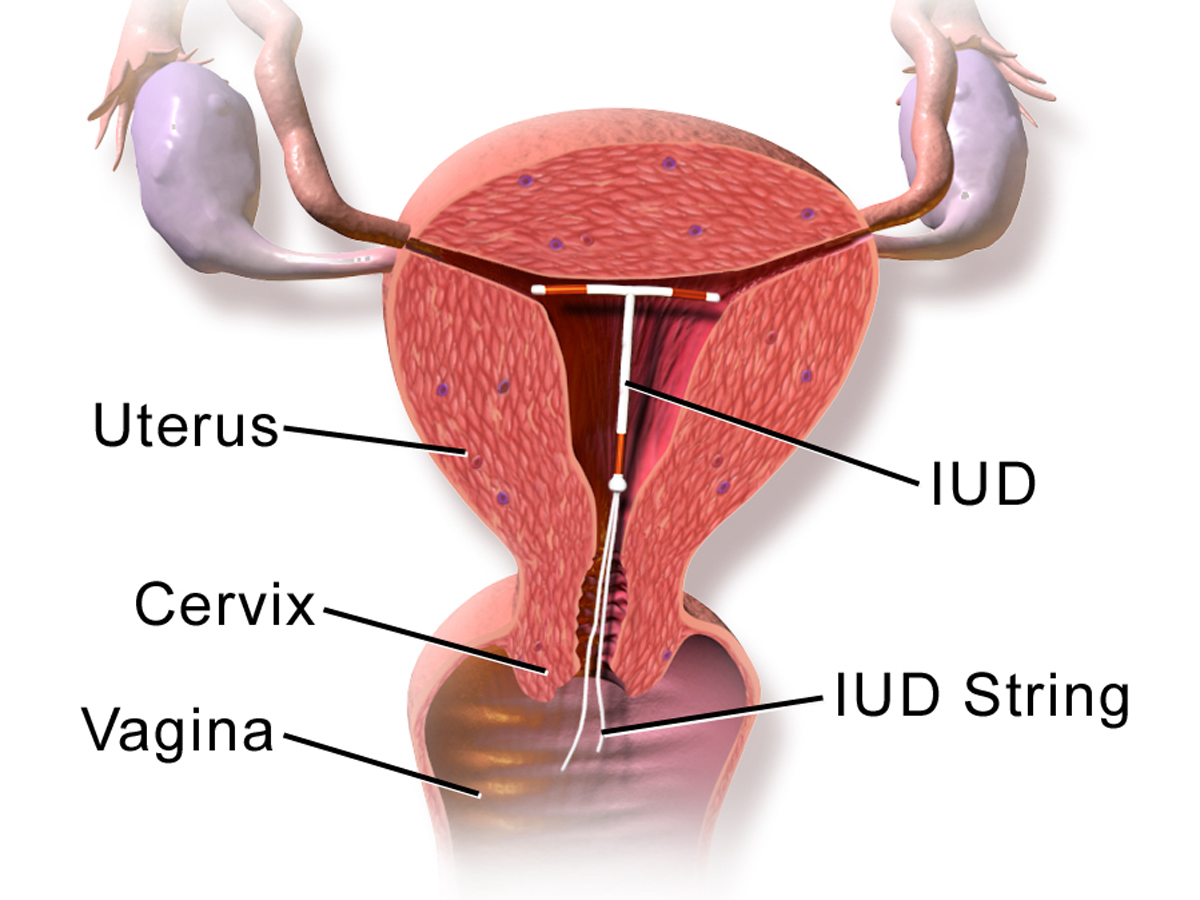
There are many contraception options available to young people. From barrier methods: condoms and internal condoms that help prevent STIs and/or pregnancy, to hormonal methods such as: the pill, the injection, the implant, the vaginal ring, the contraceptive patch, the IUS (often called ‘the coil’), to non-hormonal methods such as the IUD (often called the ‘copper coil’).
The IUD, IUS and implant are 99% effective, making them the most effective methods of contraception. The IUD can also be used as a method of emergency contraception. For more information about different methods and to find the right one for you visit www.brook.org.uk/contraception
Can you go to a sexual health clinic instead of the GP as long as it’s relevant to your genitals? Like, for BV (bacterial vaginosis), or thrush?
You don’t have to be having sex or know you have an STI to come to a sexual health clinic. Sexual health clinics can help with a wide range of issues. If you feel you are having any issues around your sexual health or your genitals you can definitely come to a sexual health clinic, to find your local clinic click here or check out the Brook website: brook.org.uk
Does contraception just have to be for the prevention of pregnancy, or can people access it for medical reasons alone?
This one entirely depends on your circumstances and the advice of a health professional, for example it is possible to take the combined pill for a few months after you have had a LARC (long-acting reversible contraception) method fitted (such as an implant or IUS/IUD) to help regulate your menstrual cycle.
Sometimes a GP might also put someone on the combined pill before they are sexually active to help with irregular or particularly painful / heavy periods as the oestrogen can help regulate and ease symptoms. In some cases of endometriosis (or other gynaecological issues) an IUS (the hormonal coil) may be fitted before someone is sexually active as it can sometimes stop periods and may ease other symptoms.
If you are seeking contraception for medical reasons it is best to see your GP rather than a sexual health clinic, as they will be able to provide a smoother monitoring service if you are put on any medication and may be more familiar with your personal medical history.
Why can’t I book in advance?
You can book in advance at Brook if you call 01179290090. You can also make appointments at central health clinic at certain times of day during the week, for more information on this go to: unitysexualhealth.co.uk/our-services/unity-clinics-opening-times
Brook also has a drop in service so waiting times are variable. There are some young people’s clinics that offer a walk-in service only such as the Amelia Nutt Young Persons Clinic, but if any of those walk in times don’t suit you, you are welcome to make an appointment at Brook or at Central Health Clinic in Bristol.
If I’m trans, do I go by my genitals or my identity?
Brook and Unity Sexual Health encourage everyone to use the name, pronouns and gender identity that they prefer. All sexual health staff should respect this, and please do let us know if you feel that that isn’t the case when you visit.
During your consultation, we might need to ask you about your genitals – this is because we sometimes use different tests according to which genitals someone has; a urine sample instead of a swab, for example. If we do this, it’s because we want to use the most appropriate and most effective tests for you as an individual, to ensure that you get accurate results. If there is particular language or words that you would like us to use, again, please do tell us – we want you to feel comfortable during your consultation.
Can you get dams at sexual health clinics or is it only condoms?
A dam is a piece of flavoured latex, which is placed over the vagina or anus when performing oral sex. In general dams are not usually offered for free at sexual health clinics. However, there will be a lot of dams being given away by UNITY sexual health at Bristol Pride Day this year (13th July), and you can easily make your own out of a flavoured condom (check out our website for instructions and for more info on why dams are useful: brook.org.uk/your-life/dental-dams) You can also buy dams online (make sure they are from a reputable store and of good quality first!)
Do clinics give out latex-free condoms?
Latex-free condoms are available for free from Brook and other sexual health clinics in Bristol, however they are only available for those who genuinely have a latex allergy, if you just have a preference for latex free condoms then you’ll need to buy those yourselves.
How long do sexual health clinics keep records for?
Brook keeps records forever, in line with government rules and guidance published after the Independent Inquiry into Child Sexual Abuse (IICSA) in 2015. We keep physical records in secure storage and any electronic records in a secure online database. UNITY Sexual Health at the Central Health Clinic keeps adult records for 8-10 years after the patient was last seen, but for young people all records are kept until their 26th birthday complying with guidelines by IICSA. After this time period records are destroyed. If you have any questions about record keeping at Brook, please email: communications@brook.org.uk.
For more information about advice about sexual health you can follow Brook on Instagram @brook_sexpositive.